In-Network vs. Out-of-Network Benefits
In-Network vs. Out-of-Network Benefits
June 12, 2020
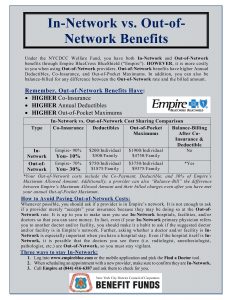 Under the NYCDCC Welfare Fund, you have both In-Network and Out-of-Network benefits through Empire BlueCross BlueShield (“Empire”). However, it is more costly to you when using Out-of-Network providers. Out-of-Network benefits have higher Annual Deductibles, Co-Insurance, and Out-of-Pocket Maximums. In addition, you can also be balance-billed for any difference between the Out-of-Network rate and the billed amount.
Under the NYCDCC Welfare Fund, you have both In-Network and Out-of-Network benefits through Empire BlueCross BlueShield (“Empire”). However, it is more costly to you when using Out-of-Network providers. Out-of-Network benefits have higher Annual Deductibles, Co-Insurance, and Out-of-Pocket Maximums. In addition, you can also be balance-billed for any difference between the Out-of-Network rate and the billed amount.
How to Avoid Paying Out-of-Network Costs:
Whenever possible, you should ask if a provider is in Empire’s network. It is not enough to ask if a provider merely “accepts” your insurance because they may be doing so at the Out-of-Network rate. It is up to you to make sure you use In-Network hospitals, facilities, and/or doctors so that you can save money. In fact, even if your In-Network primary physician refers you to another doctor and/or facility, you should make it a habit to ask if the suggested doctor and/or facility is in Empire’s network.
Further, asking whether a doctor and/or facility is In-Network is especially important when you have a hospital stay. Even if the hospital itself is In-Network, it is possible that the doctors you see there (i.e. radiologist, anesthesiologist, pathologist, etc.) are Out-of-Network, so you must stay vigilant.
Three ways to stay In-Network:
- Log into empireblue.com or the mobile application and pick the Find a Doctor tool.
- When scheduling an appointment with a new provider, make sure to confirm they are In-Network.
- Call Empire at (844) 416-6387 and ask them to check for you.